SACRAMENTO — Covered California announced the first-year results of its first-in-the nation health plan accountability program, the Quality Transformation Initiative (QTI), at its recent board meeting.
The QTI — aimed at improving health care outcomes and reducing disparities for members — was created with input from consumer advocates, health care providers and health insurance companies. It was developed in collaboration with the Department of Health Care Services and CalPERS.
The QTI establishes direct and substantial financial incentives (up to 1 percent of premium in the first year, rising to 4 percent of premium in future years) for all Covered California health insurance companies by requiring payments for failing to meet specified benchmarks for a focused, meaningful set of health-outcome measures. These equity-centered outcome measures include blood pressure and diabetes control, colorectal cancer screening and childhood immunizations.
Nearly all qualified health plan issuers saw improvement year over year in these categories in the first year of the Quality Transformation Initiative. These improvements translate to important health outcomes for Covered California enrollees: more enrollees receiving recommended cancer screenings, more children being vaccinated and more Californians able to manage their chronic conditions. Despite these improvements, Covered California will collect over $15 million from health insurance companies for not delivering the level of outcomes that the Quality Transformation Initiative holds them accountable for. These dollars will be invested back into Covered California enrollees through targeted population health investments in 2025.
“We are extremely proud of this first-in-the nation program designed to hold health plans accountable, so that Californians can get the equitable health care they all deserve,” said Dr. Monica Soni, chief medical officer of Covered California and leader of the program’s implementation team. “We wanted to select a small set of measures with high clinical impact to improve health outcomes for as many Californians as possible.”
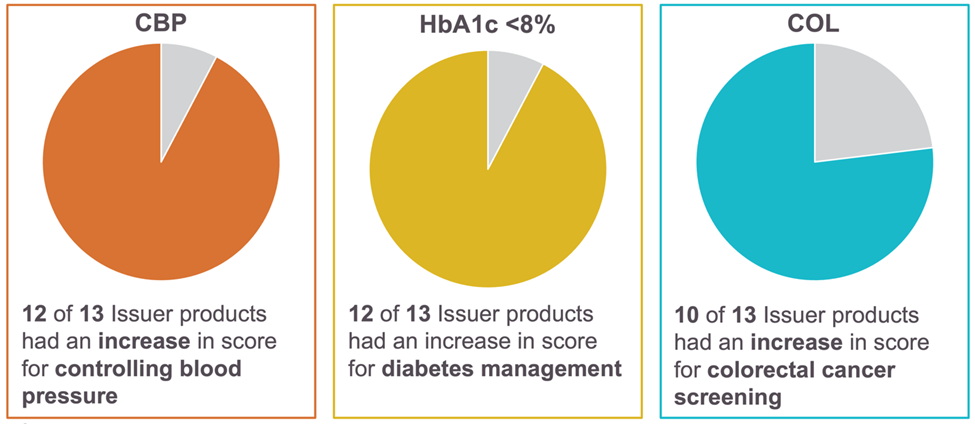
Figure 1: First year of Quality Transformation Initiative leads to health screening improvements
Covered California health plans delivered the most significant improvements for measures of chronic-condition management, with 12 of 13 issuers increasing the percentage of members controlling their high blood pressure and managing their diabetes. Overall, diabetes management improved 6 percent on average, while blood pressure control improved by 12 percent on average. Blood pressure was chosen as it is a key risk factor for cardiovascular disease (heart attacks and strokes), which is the leading cause of death in the United States. Additionally, 50 percent of Californians have diabetes or pre-diabetes, so it is a major health concern across all demographics in the state.
Ten of 13 health insurance companies also increased the rate of colorectal cancer screening among their members, at an average increase of 12 percent. Cancer is the second leading cause of death after heart disease in the United States, and colorectal cancer is the second leading cause of cancer death after lung cancer.
While some health insurance companies did improve their childhood vaccination rates, there was an average decline across the marketplace that is indicative of broader national trends in vaccination. “Childhood immunizations have decreased in the past five years, a trend that needs to be reversed and an outcome that Covered California will remain focused on,” said Dr. Soni. Childhood immunizations prevent up to 10.5 million diseases annually and for every $1 spent on immunizations, there can be as much as $29 in health care savings.
“The Quality Transformation Initiative is another example of California building upon the Affordable Care Act and making sure health care is equitable across the state,” said Covered California Executive Director Jessica Altman. “We want to thank our partners at DHCS and CalPERS for working with us to hold our health plan issuers accountable and make care equitable in California.”
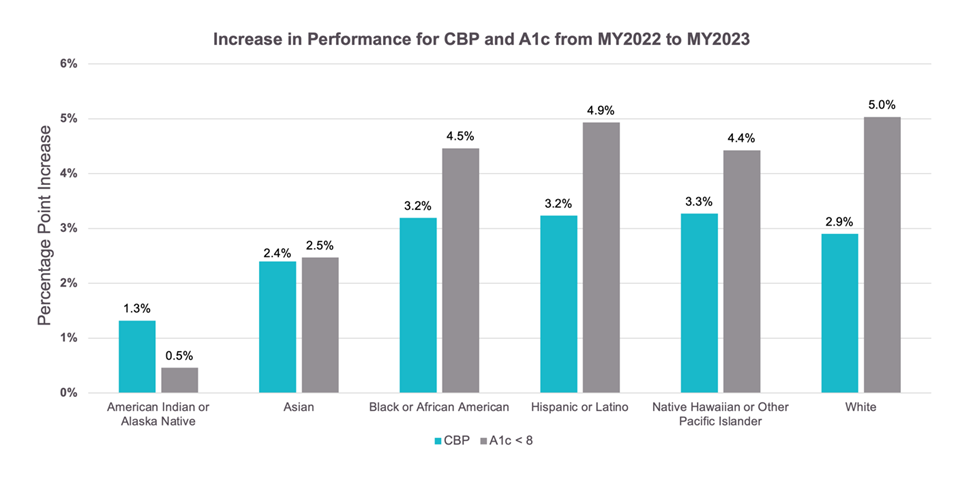
Figure 2: Performance increases across all subpopulations for diabetes and blood pressure control
For plan year 2024, up to 2 percent of premium is at risk under the Quality Transformation Initiative and may increase to up to 3 percent of premium for plan year 2025. With the rising level of financial accountability, Covered California’s health insurance companies will continue to make critical investments to improve health care outcomes for their members.
“These performance improvements are exactly what we had hoped for when creating the Quality Transformation Initiative,” Dr. Soni said. “We are optimistic the qualified health plan issuers will continue to improve each year and ultimately that all Californians will get the care they deserve.”
Figure 3: Qualified health plan issuers participating in the Quality Transformation Initiative
| PY2023 | PY2024 | PY2025 | PY2026 |
| Anthem | Anthem | Aetna | Aetna |
| Blue Shield of California | Blue Shield of California | Anthem | Anthem |
| Balance by CCHP | Balance by CCHP | Blue Shield of California | Blue Shield of California |
| Health Net | Health Net | Balance by CCHP | Balance by CCHP |
| Kaiser Permanente | Kaiser Permanente | Health Net | Health Net |
| LA Care | LA Care | Kaiser Permanente | Inland Empire Health Plan |
| Molina Healthcare | Molina Healthcare | LA Care | Kaiser Permanente |
| Sharp Health Plan | Sharp Health Plan | Molina Healthcare | LA Care |
| Valley Health Plan | Valley Health Plan | Sharp Health Plan | Molina Healthcare |
| Western Health Advantage | Western Health Advantage | Valley Health Plan | Sharp Health Plan |
| Western Health Advantage | Valley Health Plan | ||
| Western Health Advantage |































